Oncotarget published "Eltrombopag and its iron chelating properties in pediatric acute myeloid leukemia" which reported that the standard treatment for pediatric AML currently consists in a combination of cytarabine and antracycline.
Eltrombopag, a thrombopoietin receptor agonist used in immune thrombocytopenia, shows anticancer properties related to its emerging iron chelating properties.
The authors compare the anticancer effect of classically used cytarabine with DFX and ELT effects in a pediatric AML cell line, THP-1, in order to identify innovative and more effective therapeutic strategies.
ELT and DFX reduce intracellular iron concentration by inhibiting its uptake and by promoting its release.
In particular, even though further investigations are needed to better understand the exact underlying action mechanisms, this Oncotarget Research Output demonstrated that ELT improves cytarabine antineoplastic activity in pediatric AML cell lines.
This Oncotarget Research Output demonstrated that ELT improves cytarabine antineoplastic activity in pediatric AML cell lines.
Dr. Francesca Rossi from The University of Campania Luigi Vanvitelli said, "Acute myeloid leukemia (AML) represents the 20% of total childhood leukemia diagnoses [1], even though it remains the most frequent type of acute leukemia in the elderly."
The altered iron metabolism in AML patients is also strongly related to a dysregulation in the expression of iron metabolism mediators at AML cells level.
European Medicines Agency approved three iron chelators for treatment of iron overload conditions: deferoxamine generally used in thalassemia major, deferiprone and deferasirox instead indicated in leukemic patients.
It was demonstrated that ELT mobilizes iron from the intracellular compartment, thus reducing the metal availability for cancer cell metabolic processes, and proposed a shuttling mechanism when ELT and DFX are combined.
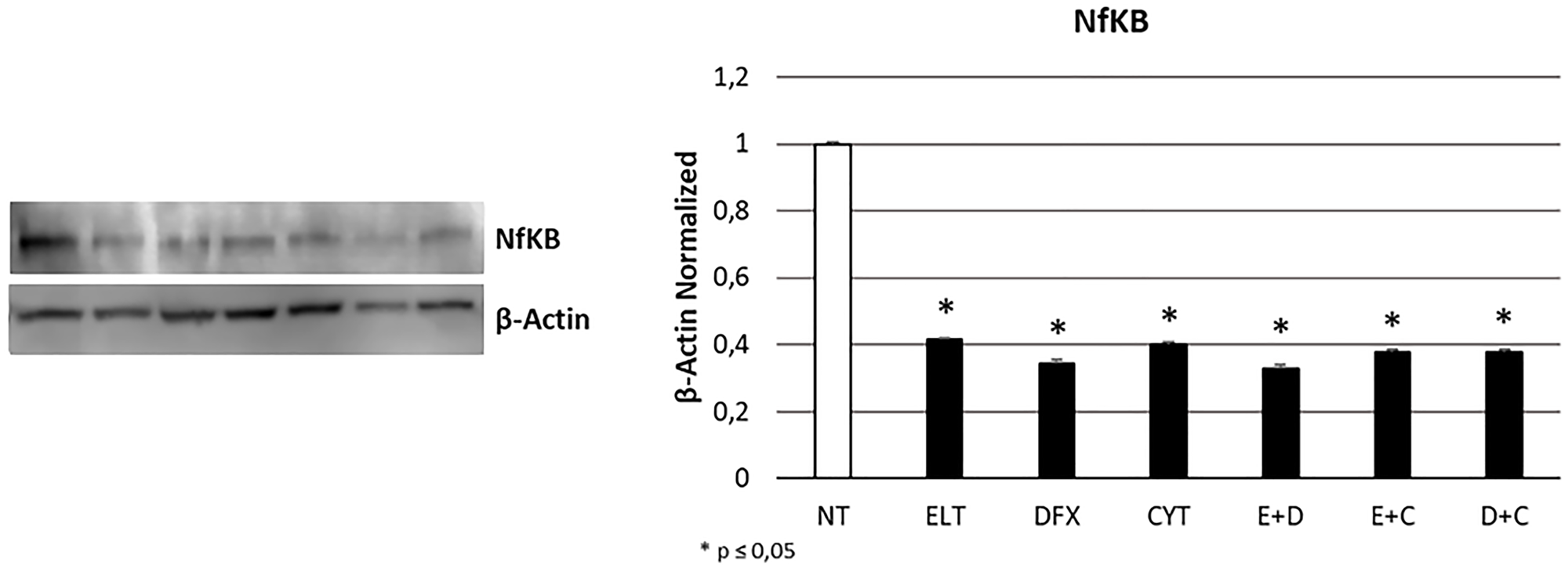
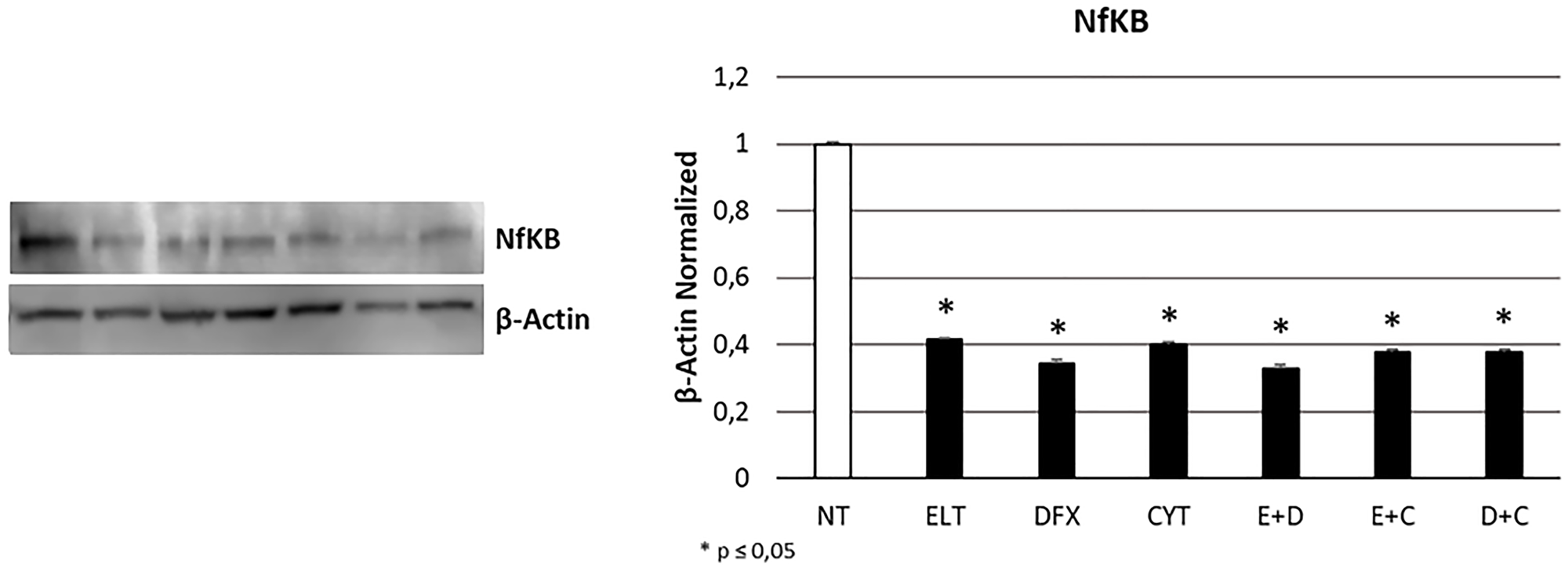
Figure 5: Effect of 48-hour treatments on proliferation. NFkB protein expression level in THP-1 cell line was determined by Western Blot, starting from 15 μg of total lysates after 48 h of exposure to ELT, DFX and Cytarabine, alone and in combination. The most representative cropped images of blots are displayed. The proteins were detected using Image Studio Digit software and the intensity ratios of immunoblots compared to that of untreated control, taken as 1 (arbitrary unit), were quantified after normalizing with respective loading controls for the housekeeping protein β-Actin. The histogram represents the relative quantification for NFkB expression as mean ± SD of three independent experiments A t-test has been used to evaluate the statistical differences in protein expression levels. * indicates p ≤ 0.05 compared to non-treated sample (NT).
In particular, ELT decreases cellular iron and further enhances iron mobilization, donating it to DFX.
In this Oncotarget study the authors tested cytarabine, the most commonly used anticancer drug in AML, with both DFX, one of the most diffused iron chelators in leukemia, and ELT, an emerging iron chelating agent, in THP-1 cell line.
The Rossi Research Team concluded, "our study lets emerge a promising synergism between ELT and cytarabine with reduction in viability, increase in apoptosis and arrest of both proliferation and cycle progression in the pediatric AML cell line THP-1. On the other hand, we can not confirm the effectiveness of DFX in AML, neither alone neither in combination with the classically used chemotherapy agent. Further investigations are certainly needed to clarify the exact mechanisms underlying the synergism between ELT and cytarabine, in particular to understand whether ELT iron chelating properties are actually responsible for these anticancer activities. However our results encourage the possibility to combine them to increase the outcome of canonic therapeutic strategy in AML, reducing dose-related side effects associated to cytarabine as well as the chemo-resistance often developed by patients against this agent."
DOI - https://doi.org/10.18632/oncotarget.28000
Full text - https://www.oncotarget.com/article/28000/text/
Correspondence to - Francesca Rossi - [email protected]
Keywords - acute monocytic leukemia, eltrombopag, deferasirox, iron chelation, cancer
About Oncotarget
Oncotarget is a bi-weekly, peer-reviewed, open access biomedical journal covering research on all aspects of oncology.
To learn more about Oncotarget, please visit https://www.oncotarget.com or connect with:
SoundCloud - https://soundcloud.com/oncotarget
Facebook - https://www.facebook.com/Oncotarget/
Twitter - https://twitter.com/oncotarget
LinkedIn - https://www.linkedin.com/company/oncotarget
Pinterest - https://www.pinterest.com/oncotarget/
Reddit - https://www.reddit.com/user/Oncotarget/
Oncotarget is published by Impact Journals, LLC please visit https://www.ImpactJournals.com or connect with @ImpactJrnls
Media Contact
[email protected]
18009220957x105